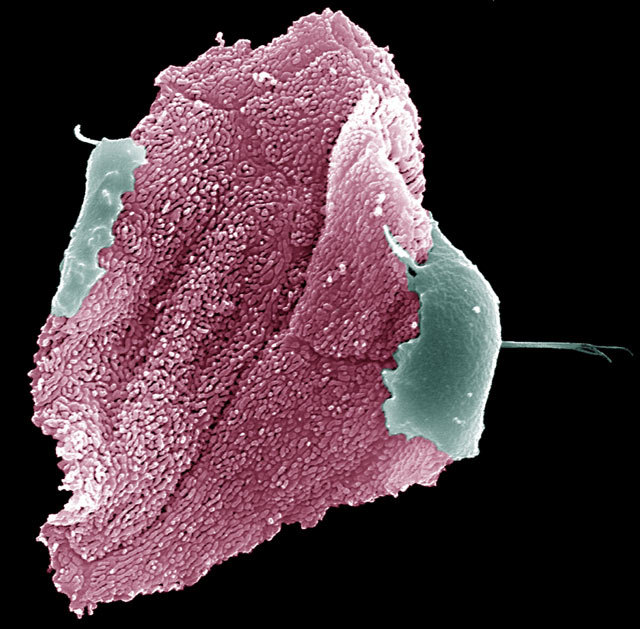
Some doctors may refer to it as the epidemic of the 21st century, yet the majority of people know very little about HPV, a highly infectious sexually transmitted disease that is linked to a wide range of cancers.
When American actor Michael Douglas announced last month that the Human Papillomavirus caused his throat cancer, he threw a long-overdue spotlight on the STI.
Spreading at pandemic levels, the virus causes almost all cervical cancer, the third most common cancer in women worldwide.
Difficult to detect without a pap smear, warning signs can go unnoticed until lesions on the cervix turn cancerous, lending it the moniker ‘the silent killer’.
In countries with a high standard of living, cervical cancer can largely be prevented through screening and treatment, says Dr Claire Ryan, a senior research officer for sexual health and diagnostics at the Centre for Biomedicine at the Burnet Institute in Australia, and a participant in a HPV prevalence study in Papua New Guinea.
“This is not the case in most resource-limited [countries], where the most efficient way to prevent or treat infectious disease is through vaccination,” said Ryan.
In 2006, America’s Food and Drug Administration (FDA) approved Gardasil, a vaccine developed to prevent cervical and genital cancer caused by HPV infections. The following year Australia became the first country to introduce a government-funded HPV Vaccination Programme to protect young women against HPV infections. The results have been “phenomenal”, according to Suzanne Garland, head of clinical microbiology and infectious diseases at the Royal Women’s Hospital, Melbourne.
By late 2012, researchers noted a 73% reduction in cancer-causing HPV infections, as well as a 90% reduction in genital warts.
“This reduction in genital warts is not only evident in those vaccinated, but also in those of vaccine-eligible-aged males and females who haven’t received the vaccination,” said Garland.
The challenge now is to bring the expensive HPV vaccine to developing countries, where 85% of the 275,000 cervical cancer-related deaths occur every year.
In May, Gavi Alliance, a public-private partnership that works to improve access to immunisation in poor countries, secured a pricing agreement with Merck and GlaxoSmithKline pharmaceutical companies that lowered the price per dose of the HPV vaccine from approximately $100 to $4.50.
Following the deal, Gavi Alliance began rolling out its year-long vaccination programme in eight countries, of which the only Asian country is Laos, where cervical cancer is the most common cancer among women aged 15 to 44.
“Laos has a high regard for women’s issues and equity in general,” said Dominique De Santis, a spokesperson for Gavi Alliance. In 2012, the country of 6.2 million applied to receive funding for the HPV demonstration project.
“Laos considers it important to introduce the vaccine as early as possible and protect young girls against this terrible cancer, and this builds on the country’s strong immunisation programme, with delivery through an integral maternal and child health approach,” said De Santis.
It is estimated that 1.8 million females above the age of 15 in Laos are at risk of developing cervical cancer. Furthermore, each year it is estimated that 317 women are diagnosed with the cancer, of which 159 will die.
Despite the lifesaving potential of the vaccine, implementation of the project is not without challenges. Girls must receive three doses within a strict six-month period, ideally before they become sexually active.
“Sound mobilisation and communication activities for immunisation programmes already exist in Laos,” said De Santis. “The success of the programme, which will initially be rolled out in one district, will rely on a strong cold chain capacity, strong routine immunisation programmes and cancer control action plans, and the ability to reach girls aged 9 to13 in and out of schools.”
Papua New Guinea, where 17.6 deaths per 100,000 are caused by cervical cancer, is one of more than 40 countries eligible for the vaccine funding in the future.
“Education and knowledge campaigns about why the three doses are important will be imperative,” said Ryan, adding that the vaccine is a preventative measure and not a replacement for regular screenings. “[In PNG we will] need to keep working to improve current screening and treatment programmes for cervical cancer, so women that will not benefit from the vaccine can access the healthcare they need.”
Despite its proven success, the long-term effects of the vaccine are still unknown.
“How long this protection will last, only time will tell. Those vaccinated earlier in trials are still showing protection [ten years later],” said Garland. “However, because of the long-term incubation period between being infected and development of cervical cancer – about 15-20 years – it is obviously going to take time to see a reduction in actual cancer cases.”
Facts about Human Papilloma Virus (HPV) and vaccine
• There are nearly 200 types of HPV
• There are between 30 and 40 types of HPV that specifically infect the genital tract and can also infect the mouth and throat
• Types 6 and 11 are directly linked to 90% of genital warts cases
• Types 16 and 18 are consistently cited as the cause of 70% of cervical cancers worldwide
• The vaccine protects people against the four above mentioned types of HPV
• Both males and females can receive the vaccine. However, women have been the primary target for funded programmes to date because of the link to minimising the risk of cervical cancer
• The vaccine should not be used in place of routine pelvic exams and Pap smears to screen for cervical cancer

